Piergiorgio Bolasco
ASL Cagliari, Italy
Title: Nutritional hypoproteic approach and phosphate control allows the Incremental Hemodialysis.
Biography
Biography: Piergiorgio Bolasco
Abstract
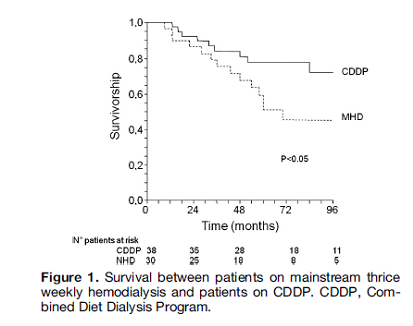
It is largely agreed that preservation of Residual Kidney Function (RKF) has a directly proportional effect on general and in particular cardiovascular mortality. The prolongation of RKF depends on a rigorous hypoproteic regimen especially in phosphate contents because of a significant output urinary phosphate that continues despite of a severe decrease of residual kidney function. The RKF>3 ml/Kg/die 1.73 sm and nutritional compliance allows to choose a new hemodialytic strategy called Infrequent Hemodialysis (ID) as both are once-weekly (CDDP) or twice-weekly hemodialysis. The nutritional regimen and phosphaturia has been frequently underestimated. The excessive proteic charge and hyperphosphataemia load and damage the residual nephrons. We compared general survival, nutritional, clinical parameters, phosphate pool balance between three patient cohorts: 10 in thrice weekly, 10 in twice weekly and 9 in once weekly hemodialysis patients. We collected over 250 urine collections in patients with RKF. The hemodialysis patients on ID who adhere accurately to a low protein diet of 0.6-0.8 g/Kg/day and phosphate intake 800-1000 mg/day were opted for the study. In view of the significant impact produced by inadequate nutrition and poor phosphate control on both RKF and the frequency of even severe cardiovascular effects, infrequent dialysis with its negative or neutral weekly phosphate balance, may constitute a valid “bridging” treatment even in the long-term. Nutritional approach and neutral phosphate control improved wellbeing and the survival rates (fig.1) compared with respect to patients receiving conventional thrice-weekly hemodialysis.